Ocular Tonometry: What It Is, Preparation And Risks
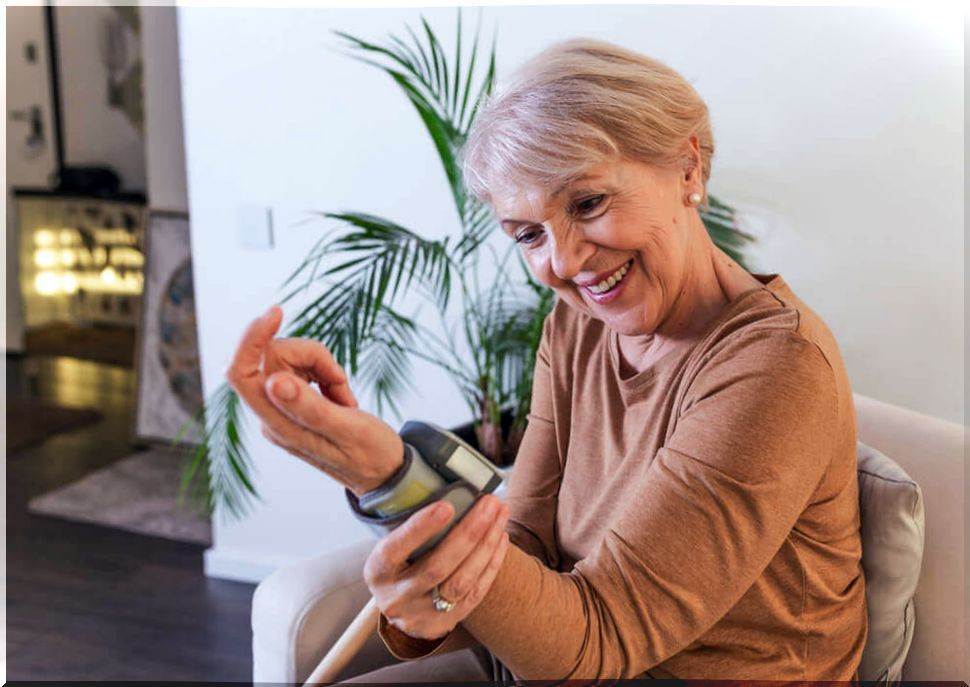
Ocular tonometry is a diagnostic test used very frequently in ophthalmology. It allows to measure the pressure levels inside the eye, that is, the so-called intraocular pressure (IOP).
Intraocular pressure is the pressure exerted by fluids from within the eye against the walls of the eye. It is a determining parameter that allows diagnosing serious pathologies such as glaucoma. This is very relevant, since if it is not treated it leads to blindness.
Ocular tonometry is a simple and safe test. However, there are different modalities and ways of doing it. In this article we explain everything you need to know.
What is an ocular tonometry?
Ocular tonometry, as we have pointed out in the introduction, is a test performed by ophthalmologists. It consists of measuring intraocular pressure. It is done indirectly, using an instrument called a tonometer .
Intraocular pressure is the pressure exerted by the fluids present within the eyeball against its walls. These liquids are the vitreous humor and the aqueous humor. The eyeball is a firm structure that cannot be overstretched.
Hence, when the amount of liquid inside increases, the pressure increases. It is considered normal when the measurement is between ten and twenty millimeters of mercury. This is explained in an article by the American Academy of Ophthalmology .
If the pressure rises above this figure, we speak of hypertension of the eye . This can damage the cells of the optic nerve. Ocular tonometry is considered the most useful test for the diagnosis of glaucoma.
However, there are factors that may condition the outcome of the study. Therefore, it is not considered a definitive test, but an estimate. One of the elements that affects the procedure is the thickness of the cornea; the thicker it is, the higher the pressure figures are likely to be.

Types of ocular tonometry
Ocular tonometry can be performed in different ways. The most widely used is the so-called Goldmann flattening tonometry. It consists of indirectly measuring pressure by placing the tonometer in a slit lamp.
The problem is that it is significantly influenced by the thickness of the cornea, as we have pointed out. For this reason, it is usually necessary to require other techniques to complement the information.
A pachymetry is often used. This is a test that allows you to measure that corneal thickness. In this way, the intraocular pressure can be better estimated. Since Goldmann tonometry is a contact technique, local anesthetics are used before it is performed.
Rebound tonometry
Rebound ocular tonometry is another modality. According to the specialists of the ISV Clinic, it uses the emission of a microscopic metallic probe to measure the pressure.
What is done is to determine the speed at which the emission of the probe stops when it hits the cornea. In this case, anesthetics are not used. Although it seems aggressive, it is actually easier to guide the diagnosis for the first time.
Pascal dynamic tonometry
This type of ocular tonometry is also contact tonometry. In recent years its use is increasing. This is because, unlike Goldmann tonometry, it is not so interfered with by the thickness of the cornea.
In this way, you do not need additional examinations. However, it is more complex to perform and takes longer to complete. That is why it is recommended that it be performed by a qualified ophthalmologist.
Pneumatic ocular tonometry
Of all the ocular tonometry techniques that we have described, pneumatics is the only one that is not contact. It consists of directing a small stream of air towards the cornea.
The idea is to quantify how much air pressure is required to flatten the surface of the cornea. This is how the intraocular pressure value is measured.
How to perform the exam?
As we have seen in the previous section, each ocular tonometry is performed differently. The choice of technique will depend on the preferences and experience of the ophthalmologist. Also of the material that you have in your consultation.
Goldmann tonometry is performed in a semi-dark room. The patient should lean on the slit lamp, sitting as still as possible. To perform it, the ophthalmologist uses anesthetic drops in each eye.
In addition, an eye drop of a dye called fluorescein is instilled . In this way, the conjunctiva is stained yellow or orange. It is a painless technique, although it can cause later discomfort.
In rebound tonometry or pneumatics the patient is also seated. You should avoid blinking, although anesthetics and fluorescein are not used. Still, both are painless.
Why is ocular tonometry performed?
Ocular tonometry helps in the diagnosis and monitoring of glaucoma. It is a pathology that damages the optic nerve, as a result of increased intraocular pressure.
It is one of the main causes of blindness in people over 60 years of age. Glaucoma has a hereditary component. In addition, people of African descent are at higher risk of suffering from it.
If not treated quickly it leads to permanent vision damage irreversibly. That is why ocular tonometry is so important. Be aware that blood pressure figures are not related to those inside the eye.
How to prepare for the exam
In order to perform an ocular tonometry, no specific preparation is required. It is a short test that usually lasts 5 or 10 minutes. Ideally, the patient should go to someone, although it is not strictly necessary.
This is because some people have trouble seeing properly after using the eye drops. Before going to the exam, the ophthalmologist must know the patient’s medical history. Especially if you suffer from any type of illness or if you take medication.
Allergies are just as important. People wearing contact lenses will need to remove them before the test. It is important that the patient is calm and does not move so that the results are not altered.
What can the results indicate?
Eye pressure is considered normal when it is between 10 and 20 millimeters of mercury. For this reason, when performing an ocular tonometry different results come out, a pathology must be suspected.
However, we must emphasize that there are factors that influence values. If it is not taken into account that the thickness of the cornea can vary the number obtained and errors can be made when interpreting the measurement.
Along with Goldmann tonometry, a pachymetry is recommended. If it is not done and the result is high, it could be due to a thicker cornea.
In any case, if the intraocular pressure is elevated it may be due to glaucoma. It can also be increased if there is blood in the anterior chamber of the eye or an injury there.
Ocular tonometry is a safe test
The truth is that all tests that have to do with the eyes can seem unpleasant at first. However, ocular tonometry is short, simple, and harmless. It does not usually create discomfort in the patient.
In addition, it allows the diagnosis and monitoring of serious pathologies such as glaucoma. However, it is recommended that it always be performed by an experienced ophthalmologist.